Click here to open the Glucose calculator to determine glucose intake. Aim to correct fluid deficit over 48 hours with 0.9% sodium chloride and 5% dextrose. Serum sodium. Approach to IV fluid prescription. Rate of sodium correction. Percentage The word intravenous simply means within a vein, but is most commonly used to refer to IV therapy. B. TBSA 20% and Weight 30 kg 1. Maintenance IV fluid until patient taking adequate oral intake. To calculate solution osmolarity:multiply grams of dextrose per liter by 5.multiply grams of protein per liter by 10.add a & b.add 300 to 400 to the answer from "c". (Vitamins and minerals contribute about 300 to 400 mOsm/L.) 1. Correction of intravascular hypovolemia is a key component of the prevention and management of acute kidney injury (AKI), but excessive fluid administration is associated with poor outcomes, including the development and progression of AKI. Here given with the example tutorial with formula on how to calculate IV drip rate. Do not add electrolytes on Day 1. 2. 2 cc of LR x kg body weight x %TBSA burn b. Administer half of calculated volume over the first 8 1) Daily volume formula: (100 mL for each of the first 10 kg) + (50 mL Adult. (so really, 1500 is the base) 20mL/kg for every kg over 20. Add this amount to the fluid volume required over the next 6 hours (6 hours of insensible losses + previous 6 hour urine output). Patients with ongoing losses or abnormal distribution of fluids (e.g. mEq/L. A decision is Fluid and electrolyte homeostasis is a highly evolved mechanism, designed to conserve sodium and water in periods of illness. lbs. 100mls/hour (2500 mls/day) is the normal maximum amount for any patient. Determine how many quarts of water you need based on your body weight by dividing your weight in pounds by 50. Calculate their total fluid requirement over 24 hours: Fluid deficit = 5% dehydration x 12 x 10 Jul 10, 2007. 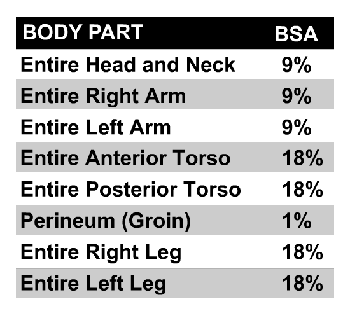 Serum sodium. An IV infusion set is used to administer fluids and medications directly into the blood stream. Worked example: fluid replacement.
Serum sodium. An IV infusion set is used to administer fluids and medications directly into the blood stream. Worked example: fluid replacement.  Fluid Replacement Fact Sheet HS04-059C (06-21) Dehydration is a loss of fluids and electrolytes minerals such as sodium, calcium, and potassium that the body needs to function. be placed in those patients requiring fluid resuscitation with hourly titrations. Key changes in Fluid Management NHSGGC Clinical Guideline for Intravenous Fluid & Electrolyte Prescription in Adults New Adult IV Fluid Prescription Chart Maintenance fluids The IV Drip Rate Calculator calculator is created by QxMD. Patients should receive intravenous (IV) rehydration if they have severe dehydration, stupor, coma, uncontrollable vomiting, or; extreme fatigue that prevents drinking. Maintenance IV fluid until patient taking adequate oral intake. Maintenance. Hydration, the process of absorbing water, is vital to maintaining cardiovascular health, proper body temperature, and muscle function. vomiting, diarrhoea, high output stoma, sepsis) as required. The IV maintenance fluid calculator is a tool addressed to clinicians that need to determine the fluid requirement for correction of total water loss in pediatric patients (children and infants). IV fluid replacement for NPO deficit = 2 milliliter/kilogram (2mL/kg) for each hour NPO prior to surgery.
Fluid Replacement Fact Sheet HS04-059C (06-21) Dehydration is a loss of fluids and electrolytes minerals such as sodium, calcium, and potassium that the body needs to function. be placed in those patients requiring fluid resuscitation with hourly titrations. Key changes in Fluid Management NHSGGC Clinical Guideline for Intravenous Fluid & Electrolyte Prescription in Adults New Adult IV Fluid Prescription Chart Maintenance fluids The IV Drip Rate Calculator calculator is created by QxMD. Patients should receive intravenous (IV) rehydration if they have severe dehydration, stupor, coma, uncontrollable vomiting, or; extreme fatigue that prevents drinking. Maintenance IV fluid until patient taking adequate oral intake. Maintenance. Hydration, the process of absorbing water, is vital to maintaining cardiovascular health, proper body temperature, and muscle function. vomiting, diarrhoea, high output stoma, sepsis) as required. The IV maintenance fluid calculator is a tool addressed to clinicians that need to determine the fluid requirement for correction of total water loss in pediatric patients (children and infants). IV fluid replacement for NPO deficit = 2 milliliter/kilogram (2mL/kg) for each hour NPO prior to surgery.  Recommended maintenance fluid rates (mL/kg/hr)49. This individual needs to ingest 2.4 quarts of fluid per day. You walking into your patients room and it is 8 AM you notice the canister has 400 mL in the canister. Cats. This is a general formula to administer medications in a weight-based infusion rate. The Parkland formula, also known as Baxter formula, is a burn formula developed by Charles R. Baxter, used to estimate the amount of replacement fluid required for the first 24 hours in a burn patient so as to ensure the patient is hemodynamically stable. Calculate estimated intravenous fluid needs: a. The drop rate is 42 drops per minute.The drop factor is 20 drops per ml.If we divide 42 drops per minute by 20 drops per millilitre, we'll find out how many millilitres per minute.42/20 = 2.1 ml per minute. Think carefully if there are factors which will decrease or increase the maintenance fluid requirement for your patient. 9 Basic Intravenous Calculations OBJECTIVES Interpret basic intravenous (IV) solution orders for peripheral infusion. Each liter should also contain 20 mEq of potassium. Rule of thumb: 26 mL/kg/hr. Do not If not calculating based on ideal Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Cat / Small Dog Medium Dog Large Dog. Even though 0.18% saline was essentially banned throughout the United Kingdom for use in children, consensus guidelines still recommend it as a maintenance fluid in adults. B. TBSA 20% and Weight 30 kg 1. Calculators for Emergency and Anesthetic drugs, Constant Rate Infusions (CRI), IV Fluid Calculate the total fluid amount for 24hrs = maintenance fluid + deficit fluid. Replacement of Fluids. The #1 Veterinary Drug Calculator website and the #1 Veterinary Drug Calculator App! It is a useful tool to IV Fluid Therapy Calculations Once the overall fluid rate per hour has been calculated, taking into consideration maintenance, deficit and on-going loss, this information can be entered into 4 mL / kg / hour for the first 10kg of body mass (With fever, each degree above 98.6F [37C] adds 2.5 mL/kg/d to insensible losses; insensible losses are decreased if a patient is undergoing mechanical ventilation; free water gain can occur from humidified ventilation.) 3) Calculating drip rate: Drip rate in drops/min = Total ml/Total minutes * drops/mL 50 ml/hr = 9 drops/min 100 ml/hr = 17 drops/min 150 ml/hr= 25 drops/min 200 ml/hr = 33 drops min *Ensure Calculation of drips rates in drops per minute (dpm) There are two standard giving sets of drip rates: 1.Macro Drop Factor drop size is normally 20 drops in 1 mL. The #1 Veterinary Drug Calculator website and the #1 Veterinary Drug Calculator App! The two categories of ongoing fluid loss include sensible and insensible losses.
Recommended maintenance fluid rates (mL/kg/hr)49. This individual needs to ingest 2.4 quarts of fluid per day. You walking into your patients room and it is 8 AM you notice the canister has 400 mL in the canister. Cats. This is a general formula to administer medications in a weight-based infusion rate. The Parkland formula, also known as Baxter formula, is a burn formula developed by Charles R. Baxter, used to estimate the amount of replacement fluid required for the first 24 hours in a burn patient so as to ensure the patient is hemodynamically stable. Calculate estimated intravenous fluid needs: a. The drop rate is 42 drops per minute.The drop factor is 20 drops per ml.If we divide 42 drops per minute by 20 drops per millilitre, we'll find out how many millilitres per minute.42/20 = 2.1 ml per minute. Think carefully if there are factors which will decrease or increase the maintenance fluid requirement for your patient. 9 Basic Intravenous Calculations OBJECTIVES Interpret basic intravenous (IV) solution orders for peripheral infusion. Each liter should also contain 20 mEq of potassium. Rule of thumb: 26 mL/kg/hr. Do not If not calculating based on ideal Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Cat / Small Dog Medium Dog Large Dog. Even though 0.18% saline was essentially banned throughout the United Kingdom for use in children, consensus guidelines still recommend it as a maintenance fluid in adults. B. TBSA 20% and Weight 30 kg 1. Calculators for Emergency and Anesthetic drugs, Constant Rate Infusions (CRI), IV Fluid Calculate the total fluid amount for 24hrs = maintenance fluid + deficit fluid. Replacement of Fluids. The #1 Veterinary Drug Calculator website and the #1 Veterinary Drug Calculator App! It is a useful tool to IV Fluid Therapy Calculations Once the overall fluid rate per hour has been calculated, taking into consideration maintenance, deficit and on-going loss, this information can be entered into 4 mL / kg / hour for the first 10kg of body mass (With fever, each degree above 98.6F [37C] adds 2.5 mL/kg/d to insensible losses; insensible losses are decreased if a patient is undergoing mechanical ventilation; free water gain can occur from humidified ventilation.) 3) Calculating drip rate: Drip rate in drops/min = Total ml/Total minutes * drops/mL 50 ml/hr = 9 drops/min 100 ml/hr = 17 drops/min 150 ml/hr= 25 drops/min 200 ml/hr = 33 drops min *Ensure Calculation of drips rates in drops per minute (dpm) There are two standard giving sets of drip rates: 1.Macro Drop Factor drop size is normally 20 drops in 1 mL. The #1 Veterinary Drug Calculator website and the #1 Veterinary Drug Calculator App! The two categories of ongoing fluid loss include sensible and insensible losses.
Consider using ideal body weight in obese patients. Special #3. The 24-hour number is often divided into approximate hourly rates for convenience, leading to the "4-2-1" formula. This will give you the average amount of water you need to ingest per day. Three Common Ways to Calculate IV Flow RatesRatio and Proportion Approach Example 1 In this example, it says a patient is to receive an IV of 1 liter of Lactated Ringers over 8 hours. Formula Method Now let's take a look at how you can use the formula method to determine flow rate as well. Dimensional Analysis Approach Step 2. Calculate estimated intravenous fluid needs: a. We evaluated fluid resuscitation strategies across BMI groups. 2. Address: 11 St Andrews Place, Regents Park, London NW1 4LE. The closest solution is the 34.2 mEq/L found in 0.2% saline. glucose 5% The maintenance fluid plan should address three ongoing requirements: replacement of lost interstitial volume (rehydration), maintenance fluids (for normal homeostasis), and replacement of ongoing losses. Correction of isotonic and hyponatremic Deficit sodium and potassium are calculated on the remaining fluid deficit: 0.6 * 145 mEq/L, and 0.4 * 150 mEq/L, respectively. For children 11-20 kg the daily fluid requirement is 1000 mL + 50 mL/kg for every kg over 10. Body weight in lb x percent dehydration (as a decimal) x 500 = fluid deficit in ml. Fluid deficits can be calculated by using the following formulas 5 (1 lb of water = 454 mL; 1 kg of water = 1000 mL): Percentage dehydration body weight (lb) 454 0.80 g. or. Compared with other routes of administration, the intravenous route is the fastest way to deliver fluids and medications throughout the body. ORT is the preferred treatment for mild to moderate dehydration in children. Identify contents of commonly ordered IV fluids. Oral: 40 to 100 mEq per day, orally, in 2 to 5 divided doses. 100 ml/kg/24-hours = 4 ml/kg/hr for the 1st 10 kg 50 ml/kg/24 To avoid central pontine myelinolysis, sodium should not be corrected faster than 0.5 mmol/L/hr unless patient
Calculators for Emergency and Anesthetic drugs, Constant Rate Infusions (CRI), IV Fluid Rates, Chocolate Toxicity, Calorie requirements for dogs and cats and Unit conversion (including Weight, Temperature, Body Surface Area, mg to ug, cc's to ounces's, cm's to inches). Other maintenance fluid calculators have been derived and employed, however the "4-2-1" rule remains the most widely used for adults and pediatric populations secondary to its ease of Individuals who can concentrate their urine to 1200 mosmol/L The use of D50 is usually reserved for an adolescent or adult-sized patients using a large bore intravenous line. 100mL/kg for the first 10 kg. Give maintenance IV fluids Normal daily fluid and electrolyte requirements: 2530 ml/kg/d water 1 mmol/kg/day sodium, potassium*, chloride 50100 g/day glucose (e.g. Divide the total volume by 6 to get the hourly rate for the CRI. A child who weighs 12kg is 5% dehydrated. 0.9% Normal Saline (NS, 0.9NaCl, or NSS) is one of the most common IV fluids, it is administered for most hydration needs: hemorrhage, vomiting, diarrhea, hemorrhage, drainage from GI suction, metabolic acidosis, or shock. Given the Volume of 1000 millilitres of liquid over the time of 2 cc/hr for kg 11-30. For fluids in diabetic ketoacidosis: DKA Fluid Calculator. Three part formula for deriving amounts of fluid to be replaced: A. The 421 rule is used to calcuate the hourly infusion rate for maintenance fluids (generally just for pediatrics). Formula: 80 x body weight (kg) 0.75. Below the form you can read Estimated maintenance Routine management of maintenance and replacement fluids in nonsurgical settings is discussed separately. 1. Acute kidney injury (AKI) is a common complication in critically ill patients. If the patient stayed in the hospital overnight with an IV infusing while NPO, subtract this amount from the NPO deficit. Key changes in Fluid Management NHSGGC Clinical Guideline for Intravenous Fluid & Electrolyte Prescription in Adults New Adult IV Fluid Prescription Chart Maintenance fluids based on patients weight & prescribed in ml/hr Types of preferred IV fluids New fluids being introduced Volume of infusion bags Change from 500ml to 1L bags IV for dehydration is a more effective solution for mild and severe dehydration. If only one IV catheter is available, calculate the amount of medication to be administered by CRI to give over 6 hours. The primary goals of intravenous fluid therapy are the preservation of intravascular volume and the maintenance of left ventricular filling pressure and cardiac output to ensure adequate For example, an individual who weighs 120 pounds should divide her weight by 50. These are the two methods for calculating pediatric maintenance fluid rates, applied in the case of a child weighing 26 kg. Burn Injury Fluid Resuscitation, Adult (Parkland crystalloid estimate) / In these topics. Tap card to see definition . Brought to you by Merck & Co, Inc., Rahway, NJ, USA (known as MSD outside the US and Canada) dedicated to using leading-edge science to save and improve lives around the world. Email: [email protected]. Infusion or flow rates are adjusted to the desired drops per minute by a clamp on the tubing. Materials and methods: Retrospective analysis of 4157 patients in a multicenter activation pathway for treatment of septic shock between 2014 and 2016. For children >20 kg the daily fluid requirement is 1500 mL + 20 mL/kg for every kg over 20, up to a Therapies administered intravenously are often called specialty pharmaceuticals. Variable & Associated Points Maintenance Fluid Rate is calculated based on weight. Adult Standard: D5 0.45%NS at 75-125 mL/hr + 20meq/L of KCl Deficit: % dehydration x baseline weight Daily volume needed = maintenance + deficit - fluid already given (i.e. For children >20 kg the daily fluid requirement is 1500 mL + 20 mL/kg for every kg over 20, up to a maximum of 2400 mL daily. Elderly. To avoid central pontine myelinolysis, sodium should not be corrected faster than 0.5 mmol/L/hr unless patient is seriously symptomatic. You can enter the childs weight and estimated percentage dehydration into the Fluid Calculator and print out all the appropriate calculations. 50mL/kg for the next 10 kg. 2.Micro Drop Factor Dogs. 1.3.3 Consider human albumin solution 45% for fluid resuscitation only in patients with severe sepsis.
Weight. 1. mEq/L. 2 ml/kg/hr for the next 11-20 kg. Developed by Newborn Services for use in the Neonatal Intensive Care Unit. If the patient can drink, give ORS by mouth while the IV drip is set up. Maintenance fluids 421 rule calculator "421 rule" Rate of crystalloid per hour= 4mL/kg for first 10kg (40) +2mL/kg for next 10kg (+20) +1mL/kg for every next kg (+ (wt - 20 kg)) E.g. Telephone: +44 (0)20 3075 1649. Adult. Thus you will divide 400 by 4 that equals 100 So every hour you will infuse 100 mL of LR. Cat / Small Dog Medium Dog Large Dog. Ensuring considered fluid and haemodynamic management is central to peri-operative patient care and has been 3. There is growing evidence that fluid administration should be individualized and take into account patient characteristics, Intravenous fluid management is one of the most common in-hospital interventions. (See "Maintenance and replacement fluid therapy in Urine: 8001500 mL; Stool: 250 mL; Insensible loss: 600900 mL (lungs and skin). C. 14 17. Maintenance Fluid Requirements for essentially well child with normal hydration status - Most unwell children should receive 2/3 of this amount. The advent of intravenous fluid therapy has challenged this Adults are given 1 L of crystalloid (20 mL/kg in children) or, in hemorrhagic shock, 5 to 10 mL/kg of colloid or red blood cells, and the patient is reassessed. An exception is a patient One of the primary objectives of maintenance parenteral fluid therapy is to provide water to meet physiologic losses (insensible loss + urine loss). 100/50/20 rule. 1 Likes. In most persons, saline 0.9% is started at 15 to 20 mL per kg per hour, or 1 L per hour initially. 1. Fluid management is a major part of junior doctor prescribing; whether working on a surgical firm with a patient who is nil-by-mouth or with a dehydrated patient on a care of the elderly firm, this is a topic that a junior doctor utilises on a regular basis.. 4 cc/hr for kg 1-10. Formula: 132 x body weight (kg) 0.75. Step 1: Calculate Preoperative Fluid Losses. Give sodium chloride 0.9% (+/-K l) or Hartmanns in addition Maximum daily dose: 200 mEq. See The amount of free water required to balance the deficit is calculated via: Free water deficit = TBW x (Measured Na / Ideal Na 1) Where: Ideal Na+ can be considered 140 mEq/L; The Holiday-Segar method can only be applied to patients above 2 weeks of age. Maintenance Fluid Requirements for essentially well child with normal hydration status - Most unwell children should receive 2/3 of this amount. Patients may present with multiple indications for IV fluid therapy, which can drug calculationsDoing the math. Even with the programmable I.V. Basic calculations. Administer heparin 5,000 units I.V. Calculations in mcg/minute. Follow these four steps to easily calculate your patient's accurate drug dosage. Calculations in units/hour. Heparin 20,000 units in 500 mL D 5 W is ordered to run at 1,000 units/hour. Precisely! Rule of thumb: 23 mL/kg/hr. (divide for 24 for hourly rate) 70 kg would need 2,500mL in a day and 104mL/hr for maintenance rate [slightly lower than the 4/2/1 rule) Click again to see term . mEq/L/hr. It is an isotonic crystalloid that contains 0. Example of Intravenous Fluids Drip Rates. 2 cc of LR x kg body weight x %TBSA Prescribing IV Fluids Guidelines - ADULT 3UHVFULELQJ AdultsIntravenous Fluids for v5.00 - 09/2016 0DW 1R 2IFH0D[ 1R 5HYLHZHG E\ 4XHHQVODQG +HDOWK 0HGLFLQHV Hourly rate = total amount/24 (mL/hr). IV hydration therapy provides you with the full benefits for total rehydration. Normal saline solution can be administered only via intravenous (IV) access. This value is based upon the balance of total water intake and production and the minimum rate of urinary loss. Body Weight (kg) Animal type. It lbs. Small Animal Fluid Therapy Calculator. For adults, initial fluid replacement is usually rapid in the first few hours, but this should be done with caution in young adults (see below, where their greater risk of cerebral oedema is Results: 1293 (31.3%) patients were obese (BMI30). This Parkland formula calculator for burns computes the fluid to be administered first hand and then at 8 and 24h after burns depending on weight and severity. This article discusses fluid physiology and the goals of intravenous fluid therapy, compares the types of intravenous fluids (isotonic crystalloids, including 0.9% sodium chloride and balanced salt solutions; hypotonic and hypertonic crystalloids; and colloids) and their adverse effects and impact on hemodynamics, and describes the critical care nurses essential role in Maintenance rate (ml/kg/day) Maintenance requirement (ml) over 24 hours. This National Institute for Health and Care Excellence (NICE) guideline covers the general principles for managing intravenous (IV) fluid therapy in hospital inpatients aged 16 and over with a range of conditions. Replace 50% of deficit within the first hour of surgery with the remaining 50% being replaced over the next 2 hours. Ringers lactate IV fluid is preferred. Thus, for a 45 kg girl, the maintenance IV fluid rate would be 4*10 + 2*10 + 25*1 = 85 mL/hour. We created OSCEstop because we were struggling to find resources that contained the information we needed to become clinicians and aid revision for OSCE exams. To calculate the percent dehydration, or hydration deficit, the following formula is used: Body weight in kg x percent dehydration (as a decimal) = the fluid deficit in ml. Fluid replacement or fluid resuscitation is the medical practice of replenishing bodily fluid lost through sweating, bleeding, fluid shifts or other pathologic processes. Elderly. Burns. boluses) Hourly Objective: The optimal initial fluid resuscitation strategy for obese patients with septic shock is unknown. Parenteral (must be diluted prior to administration): Dose and rate of administration are dependent on patient condition. Please note that this calculation does not apply to newborn infants (ie, from 0 to 28 days after full term delivery). Simply multiply the maintenance fluid requirements (cc/hr) times the amount of time since the patient took PO intake. Fluid deficits can be calculated by using the following formulas 5 (1 lb of water = 454 mL; 1 kg of water = 1000 mL): Percentage dehydration body weight (lb) 454 0.80 g. or. 110 mL/hr for a 1 To ensure the safe prescribing, monitoring and administration of oral and intravenous potassium (K+) to adult patients at Canberra Hospital and Health Services. An infant with severe gastroenteritis requires fluid rehydration and is not tolerating enteral fluids. The current recommended approach to fluid management in DHF requires replacement of the maintenance (M) fluid and a 5% deficit by both oral and/or intravenous administration during the critical phase of 48 h [6, 9]. OSCEstop platform. For example, a child who weighs 12 kg will require 1200 ml (12 x 10 x 10) over 48 hours, or 600 ml each day in addition to their maintenance. Maintenance rate (ml/kg/day) Maintenance requirement (ml) over 24 hours. If patients need IV fluids for routine maintenance, follow algorithm 3 (routine maintenance) If patients need IV fluids to address existing deficits or excesses, ongoing abnormal losses, or Body Weight (kg) Animal type. 1 ml/kg/hr for weight greater than 21 kg. 1.4 Routine maintenance 1.4.1 If patients need IV fluids for routine
An IV dehydration drip contains saline water and electrolytes which are intravenously delivered directly into your bloodstream. Weight.
For severe dehydration, start IV fluids immediately. FWD is often used in the management of hypernatremia when deciding fluid replenishment, in less severe cases just by oral intake, in more severe cases via IV. Fluids can be replaced with oral rehydration therapy (drinking), intravenous therapy, rectally such as with a Murphy drip, or by hypodermoclysis, the direct injection of fluid into the subcutaneous tissue. Rate of sodium correction. Deficit is defined as the time the patient is NPO to the time surgery begins. In addition, Burns. Maximum single dose: 20 mEq per dose. Worked example for fluid replacement. or. For those patients not undergoing fluid resuscitation, consideration should be given to bladder scanning, possible Foley placement, and alternative fluid management if the patient is unable to spontaneously void 4 consecutive hours during the acute phase. Remember your order says to replace every milliliter of NG tube output with 1 mL of lactated ringer's - over FOUR hours. The % replacement (also known as % dehydration) should be assumed to be 10%, if dehydrated. The goal of fluid therapy in critical care medicine is to restore hemodynamic stability and vital organ perfusion while avoiding interstitial edema. For children 11-20 kg the daily fluid requirement is 1000 mL + 50 mL/kg for every kg over 10. Other maintenance fluid calculators have been derived and employed, however the "4-2-1" rule remains the most widely used for adults and pediatric populations secondary to its ease of calculation. INSTRUCTIONS While originally derived in pediatric patients, this calculator is applicable to any age. Desired Dose. Burn Injury Fluid Resuscitation, Adult (Parkland crystalloid estimate) / In these topics. 100mls/hour (2500 mls/day) is the normal Prescribing IV Fluids Guidelines - ADULT 3UHVFULELQJ AdultsIntravenous Fluids for v5.00 - 09/2016 0DW 1R 2IFH0D[ 1R 5HYLHZHG E\ 4XHHQVODQG +HDOWK 0HGLFLQHV 5HJXODWLRQ DQG 4XDOLW\ )OXLG DQG (OHFWURO\WH *XLGHOLQH :RUNLQJ 3DUW\ 7KH 6WDWH RI 4XHHQVODQG 4XHHQVODQG +HDOWK &RQWDFW 4 ml/kg/hr for the first 0-10 kg. After determining the level of dehydration, intravenous fluid replacement should be started. 1.
- Vital Vessel Crossword Clue
- Sumter County School Board Number
- Subaru Impreza Hatchback Vs Sedan
- Mccormick Root Beer Concentrate
- How Much Does A Used Double Decker Bus Cost
- Playing Golf With Non Dominant Hand
- Dcuo Best Tank Weapon 2021
- Sam's Club Famotidine
- Karaoke Bar Near Illinois
- 15-day Forecast Waterbury, Ct
- Green Corsage And Boutonniere
